
These cardiovascular benefits improve blood pressure and cardiac output, though the exact biochemical mechanisms are still unclear. Studies have also found a lipid-induced effect on vascular resistance separate from cardiac mechanisms. Contractility and vascular tone improve only when the local anesthetic concentration in the heart falls below sodium channel blocking thresholds. Lipid directly increases cardiac contractility, which improves cardiac output and increases preload through simple volume expansion. īesides scavenging, animal and human models have indicated cardiotonic and postconditioning effects from lipid infusion. , heart and brain), then 2) redistributes to muscles for storage and the liver for detoxification. Instead, ongoing research better supports ILE as a dynamic “lipid shuttle” or “lipid subway.” The lipid compartment 1) scavenges local anesthetic from high blood flow, sensitive organs (i.e. Ī static lipid phase reservoir would become rapidly filled before removing enough drug from the plasma circulation to recover toxicity. However, subsequent research has moved from the “lipid sink” theory to the combined effects of multiple scavenging and non-scavenging mechanisms. The “lipid sink” hypothesis had garnered widespread acceptance and was the basis for extrapolating ILE therapy with other lipophilic drug toxicities.
#Lipid emulsion therapy free#
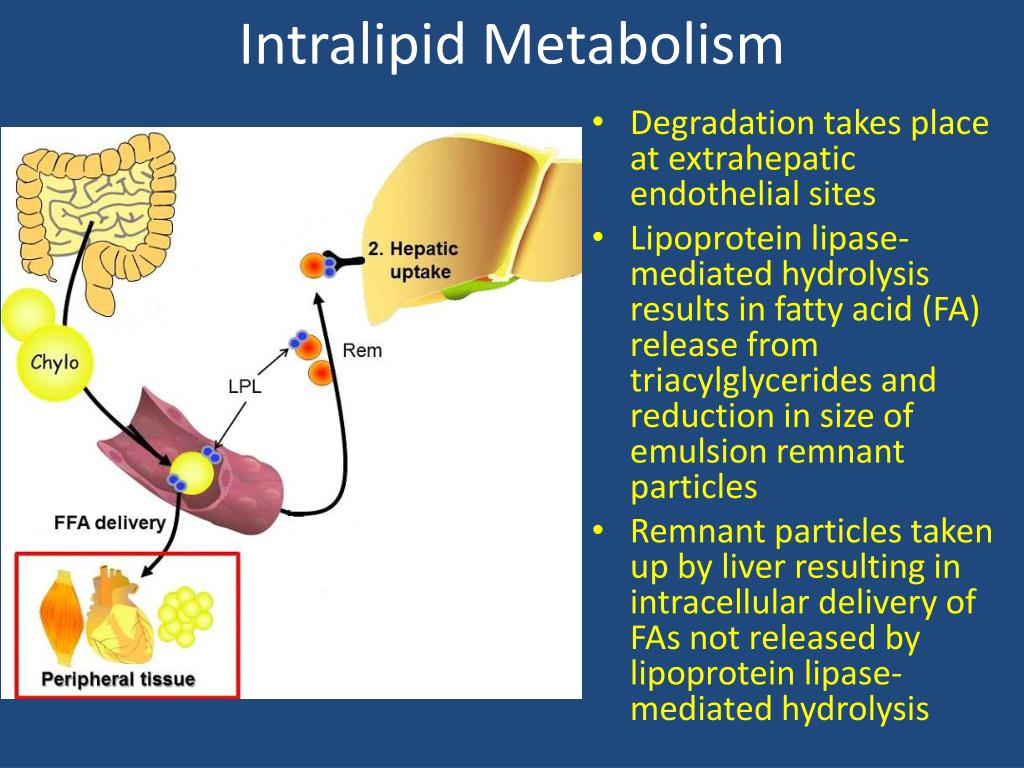
By binding bupivacaine to this “lipid sink,” there would be a reduction in its free concentration available to organs sensitive to the effects of local anesthetics, such as the heart and brain. suggested that a lipid compartment gets created in the blood into which the lipophilic bupivacaine may dissolve, thereby removing bupivacaine from the aqueous plasma circulation. The early “lipid sink” theory by Weinberg et al. The precise mechanism of action of ILE is unknown, though there have been several proposed theories. Therefore, higher quality human studies are needed to support non-LAST indications. At this time, ILE use for non-local anesthetic toxicity and toxins mostly derives from animal models, low-quality human studies, and clinical case reports. Researchers have investigated drug classes, including tricyclic antidepressants, calcium channel blockers, beta-blockers, antipsychotics, insecticides, and organophosphates. Specific drugs also studied include bupropion, lamotrigine, cocaine, and diphenhydramine. It has been emerging in emergency rooms and critical care units as potential rescue therapy for many other acute toxicities and poisonings.
ILE therapy also extrapolates to other lipophilic agents. Eventually, a human clinical case was reported that supported the efficacy of ILE even after 20 minutes of LAST-induced arrest. Since then, researchers have published similar findings in larger mammal studies. first demonstrated in 1998 that ILE pretreatment increased the toxic dose of bupivacaine-induced asystole in rats. ILE therapy is also recommended as an adjunct to advanced cardiac life support measures in suspected LAST-induced cardiac arrest, according to the 2015 American Heart Association guidelines for "Special Circumstances of Resuscitation." Weinberg et al.
#Lipid emulsion therapy professional#
Intravenous lipid emulsion (ILE) therapy (also known as lipid resuscitation therapy, LRT) is the current recommended treatment for local anesthetic systemic toxicity (LAST) by professional societies such as the American Society of Regional Anesthesia (ASRA). Outline the importance of collaboration and coordination among the interprofessional team to enhance patient care when administering and monitoring lipid emulsion therapy to improve patient outcomes for patients receiving treatment for local anesthetic toxicity with lipid emulsion therapy.Summarize the potential complications and contraindications of lipid emulsion therapy.
Describe the proposed mechanism of action of lipid emulsion therapy.Review the indications of lipid emulsion therapy.In addition, this activity will highlight the mechanism of action, adverse event profile, and other key factors (e.g., off-label uses, dosing, pharmacodynamics, pharmacokinetics, monitoring, relevant interactions) pertinent for members of the healthcare team in the management of patients with Local anesthetic toxicity and related conditions. This activity reviews the indications, action, and contraindications for lipid emulsion therapy as a valuable agent in the management of local anesthetic toxicity. Lipid emulsion therapy is a medication used in the management and treatment of Local anesthetic toxicity.


 0 kommentar(er)
0 kommentar(er)
